Healthcare digital transformation efforts are failing
After years of companies undergoing business transformation and finding only moderate success, organizations face the challenge of uncovering why healthcare digital transformations are not working. One reason these initiatives don’t deliver on their transformation promise is due to a fractured approach between strategy and the change/technology enablement necessary to adapt as the plan is implemented.
In a recent study, McKinsey found success rates of transformation efforts to be staggeringly low. In digitally savvy industries (high tech, media, and telecom), the success rate is less than 26%. In more traditional industries, including pharmaceuticals and healthcare, success rates of digital transformation fall between 4-11%.
According to a survey of U.S. hospitals and health systems, less than 30% believe that their organization is providing a best-in-class digital experience to patients.
What contributes to such dismal results?
Complexity, confusion, & frustration
Stating the tragically obvious, the healthcare system and patient care landscape is more complicated than ever.
Healthcare is fragmented. People with chronic conditions see multiple physicians and specialists in a year. Those professionals have little if any interaction with each other. Chronic conditions represent more than 80 cents of every dollar spent on healthcare, and the AMA sees the need to realign the health system around the need to prevent and treat chronic disease as one of the highest priorities.
Unconnected patient and medical records systems inhibit information sharing. The issue of data liquidity is acute. It impacts patient experience, outcomes, delivery efficiency, and quality of work for staff. Paperwork and regulatory burdens contribute to staff frustration and burnout. A variety of payment and insurance systems adds to the confusion — for both patients and caregivers.
Even the structure of staffing contributes to the fragmentation. According to a Jackson Healthcare survey of physicians:
- 21% of physicians in all specialties are employed by a hospital
- 14% are employed in a single or multi-specialty owned by a hospital
- 14% are employed by a privately owned single or multi-specialty clinic
- 9% are employed as independent contractors or Locums
This impacts how buying decisions are made, who is involved in the process, and how the staff experience is prioritized in digital transformation.
COVID-19 has only ratcheted up the stress on the system and the people on the front lines. Many predicted the possibility of a pandemic, but few if any organizations were funded, staffed, and prepared for the heartbreaking reality of 2020.
The pandemic has also increased the visibility of implicit bias and systemic inequities that are responsible for poorer patient outcomes in Black and Brown communities.
Opportunities
For most organizations, the goals of healthcare digital transformation efforts include:
- Better patient outcomes
- Staff retention and wellness
- Reduced health system costs
- Improved capacity for innovation
Through approaches and tools like automated administrative and clinical processes and smart digital platforms, there have been improvements and innovations in the past few years. Effective and consistent digital transformation has been sporadic, however, with fewer success stories than we all had hoped for.
So how do we increase the likelihood of transformations that lead to an integrated approach to patient care, better collaboration, improved hospital and clinic efficiency, and staff wellness?
McKinsey identified a list of factors that foster transformation success:
- Having the right, digital-savvy leaders in place
- Building capabilities for the workforce of the future
- Empowering people to work in new ways
- Giving day-to-day tools a digital upgrade
- Communicating frequently via traditional and digital methods
We’ve found that, strategically, this requires uniting people, process, and technology into programs that enable change and empower people.
Workforce of the future
Building capabilities and empowering people includes new and better tools, but it also requires organizations to embrace mindsets like iteration, risk-taking, innovation, and collaboration. How organizations make room for and develop these skills, and integrate them into their broader hiring and talent development programs, will drive the productivity and wellness of their teams.
Near the top of the AMA’s critical priorities is training the workforce for the challenges of the 21st century. Without alignment on what those challenges are for an organization, it’s impossible to define the path of change.
Developing the caregivers and professionals of the future is more than creating training programs. It demands that organizations change the way they think about their people. In Work Like a Boss, Nancy Lyons writes “We have to redirect our energy from conforming and enforcing conformity to accepting, supporting, and harnessing all the ways people can be themselves.”
Digital & technology
Organizations that succeed deploy more technologies to enable transformation and empower their people. From self-service and collaborative tools to big data architecture to IoT (Internet of Things) and AI (Artificial Intelligence).
Silos prevent departments from working with each other to systematically and collaboratively deliver a cohesive customer experience. To break down these silos, internal and external customer experiences are elevated by integrated business ecosystems. With an organization-wide focus on the business model and experience mapping to best understand omnichannel demands, remarkable transformation is possible.
Equity & inclusion
It is critical to develop proactive approaches to increase equity in the care and experience of all patients and healthcare workers. Often, companies do not have the experience, perspective, or expertise to make real and lasting change. If they did, they would have. Partnering with organizations specializing in equity transformation is essential.
The Center for Economic Inclusion advances inclusive growth “by elevating data-driven promising practices, advocating inclusive policies, coordinating cross-sector, community-driven development, and piloting strategies that truly close the gap.” These are the kind of approaches that are critical to making true change in healthcare for Black and Brown communities.
Doing right should be enough, but the ROI on equity and inclusion is inarguable. Reports by organizations including Mercer, Harvard Business Review, Forbes, and McKinsey prove the revenue, productivity, and innovation benefits of equity and inclusion.
Change enablement roadmap
There’s limited value in creating a strategic plan without a parallel focus on making it real. Transformation isn’t easy. It’s challenging to break habits, align differing perspectives, and establish a new, unified direction. And even when people see the need and agree with the direction, making a change is still hard. Focusing on adoption of the plan is key to ROI.
Success is riding on people adopting new mindsets and ways of working as we face a new era of our business. If they don’t, we won’t see the innovation, customization, or new revenue opportunities we’re hoping for.
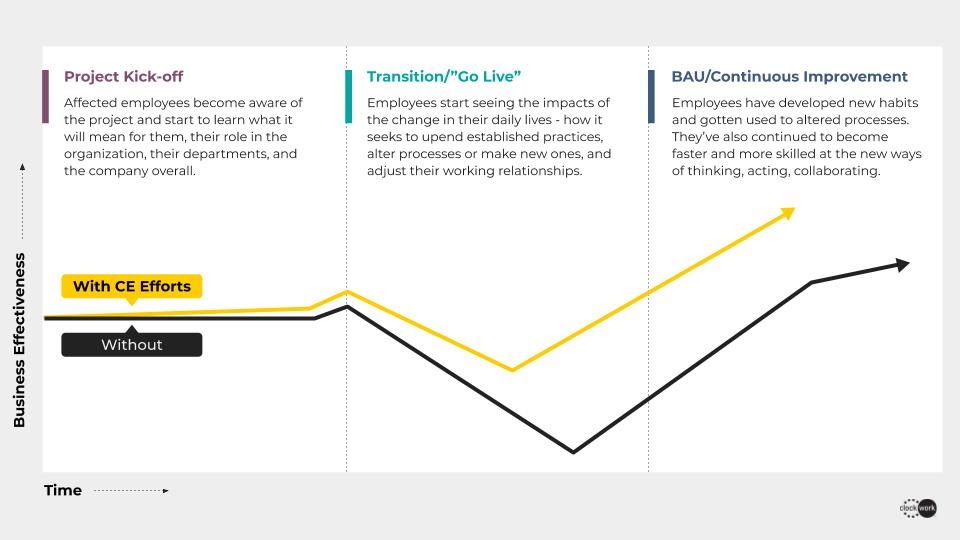
Change enablement techniques will make the difference. With efforts to make people aware of, eager, and ready for their role in adopting a new way of working, healthcare organizations reduce the productivity dip (and possibly the flight risk) that comes with change. Without change enablement practices, organizations can expect a much slower (and possibly less robust) return on investment.
Showing up for the future
2020 was a year of disruption. Now, we get to decide if we will be drivers of disruption or simply react to it. This year has shown organizations that they can change very quickly when necessary. But maintaining this level of change and adoption is more complicated. Every company will need to find sustainable but fast-paced pathways for innovation in a post-crisis environment. Amid the fear and uncertainty, people are energized as healthcare organizations make good on purpose statements, eliminate bureaucracy, empower previously untested leaders with significant responsibilities, and ‘turbocharge’ decision making. The pandemic has shown us disruption is real; now, we decide how we show up for the future.




